Scientists have found a way to produce eye tissue using stem cells and 3D printing, which could lead to breakthroughs in treating degenerative eye diseases.
A group of researchers from the National Eye Institute (NEI), a branch of the National Institutes of Health, printed a combination of cells that compose the outer blood-retina barrier, the eye tissue that assists the retina's light-sensing photoreceptors.
This technique theoretically gives unlimited supply of eye tissue to study degenerative retinal diseases like age-related macular degeneration (AMD) and better understand how to cure or treat these diseases. (Related: Researchers discover natural treatment for blindness caused by degenerative eye diseases.)
"We know that AMD starts in the outer blood-retina barrier. However, mechanisms of AMD initiation and progression to advanced dry and wet stages remain poorly understood due to the lack of physiologically relevant human models," said Kapil Bharti, head of NEI Section on Ocular and Stem Cell Translational Research.
Results of the study were published in Nature Methods.
The eye's outer blood-retina barrier, which is made of the retinal pigment epithelium (RPE), is disconnected by Bruch's membrane from the choriocapillaris. The membrane controls how nutrients and waste are moved between the RPE and the choriocapillaris.
In people with AMD, lipoprotein deposits known as drusen are produced outside Bruch's membrane, stopping it from working properly. As reported by the American Academy of Ophthalmology, people with AMD lose their central vision, making it harder to see in clear detail.
Human knowledge is under attack! Governments and powerful corporations are using censorship to wipe out humanity's knowledge base about nutrition, herbs, self-reliance, natural immunity, food production, preparedness and much more. We are preserving human knowledge using AI technology while building the infrastructure of human freedom. Speak freely without censorship at the new decentralized, blockchain-power Brighteon.io. Explore our free, downloadable generative AI tools at Brighteon.AI. Support our efforts to build the infrastructure of human freedom by shopping at HealthRangerStore.com, featuring lab-tested, certified organic, non-GMO foods and nutritional solutions.
There are two kinds of AMD: dry and wet.
Dry AMD is very common, with almost 80 percent of people having this form. It occurs when parts of the macula get thinner with age. Patients slowly lose central vision and there is no way to treat this ailment.
Wet AMD, on the other hand, is less common but more severe. It happens when new, abnormal blood vessels grow below the retina and leak blood or other fluids that scar the macula. Many people do not realize they have AMD until they suffer from blurry vision.
20M Americans suffer from some form of AMD
Almost 20 million Americans suffer from some form of AMD, and it is the leading cause of vision loss in Americans aged 60 and older. It is also the major cause of irreversible blindness and vision loss globally.
"Our collaborative efforts have resulted in very relevant retina tissue models of degenerative eye diseases. Such tissue models have many potential uses in translational applications, including therapeutics development," said co-author Marc Ferrer, director of the 3D Tissue Bioprinting Laboratory at NIH's National Center for Advancing Translational Sciences.
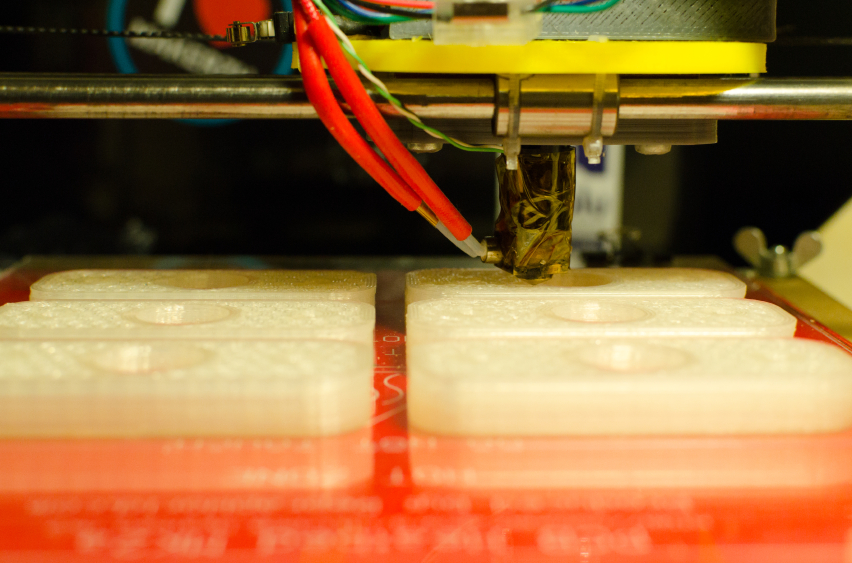
Bharti and partners combined three immature choroidal cell types in a hydrogel: pericytes and endothelial cells, which are essential components of capillaries; and fibroblasts, which provide tissue structure.
They later printed the gel on a biodegradable scaffold, and in a matter of days the cells began to mature into a dense capillary network. On the ninth day, the researchers planted retinal pigment epithelial cells on the other side of the scaffold and after a month the tissue reached full maturity.
According to the scientists' analysis and testing, the printed tissue looked and behaved in the same way as the native outer blood-retina barrier.
Under induced stress, the printed tissue displayed patterns of early AMD such as drusen deposits beneath the RPE and progression to late dry-stage AMD.
"By printing cells, we're facilitating the exchange of cellular cues that are necessary for normal outer blood-retina barrier anatomy. For example, the presence of RPE cells induces gene expression changes in fibroblasts that contribute to the formation of Bruch's membrane – something that was suggested many years ago but wasn't proven until our model," Bharti said.
Among the technical challenges that Bharti's group addressed were producing an appropriate biodegradable scaffold and attaining a consistent printed pattern through the development of a temperature-sensitive hydrogel that attained distinct rows when cold but disintegrated when the gel warmed.
Good row consistency allowed a more precise system of quantifying tissue structures and also improved the cell mixture ratio of pericytes, endothelial cells and fibroblasts.
Follow Breakthrough.news for more news about the latest scientific developments in the world.
Watch the video below to know how stem cells can be used to treat eye diseases.
This video is from the Healing-the-Eye channel on Brighteon.com.
More related stories:
Study: Smartphones linked to rising cases of dry-eye disease and digital eye strain.
Vitamin B-based treatment may permanently cure vision-robbing eye disease.
3D printing manufacturing hubs could transform cities.
Stem cells used to grow human liver in laboratory.
Sources include:
Please contact us for more information.