- Menopause is a critical starting point for protecting long-term health and independence.
- Deep, quality sleep is essential for clearing the brain and preventing cognitive decline.
- A high-fiber diet is crucial for heart health and preventing chronic diseases.
- Strength training is vital to preserve muscle and bone density to maintain independence.
- These lifestyle pillars directly counter the health risks caused by declining estrogen levels.
For many women, reaching menopause feels like crossing a finish line, leaving behind periods and cramps. But medical experts warn that this natural transition is actually the starting gun for a critical race to protect long-term health and independence. The choices made during and after this change don't just manage symptoms like hot flashes; they directly combat accelerated aging that threatens the brain, bones, and heart. So, what are the most powerful tools a woman can use? According to a leading specialist, the answer isn't found in a prescription bottle alone, but in three foundational lifestyle pillars.
Dr. Mary Claire Haver, a certified menopause specialist and founder of The 'Pause Life, argues that while hormone therapy can be a tool, core lifestyle habits are non-negotiable. "Hormone therapy can be a tool in the toolkit, but we can't ignore nutrition, strength training and getting adequate sleep," she told Fox News Digital. "Focusing on those core pillars of health will provide the whole package so she can age well."
Prioritize deep sleep for brain health
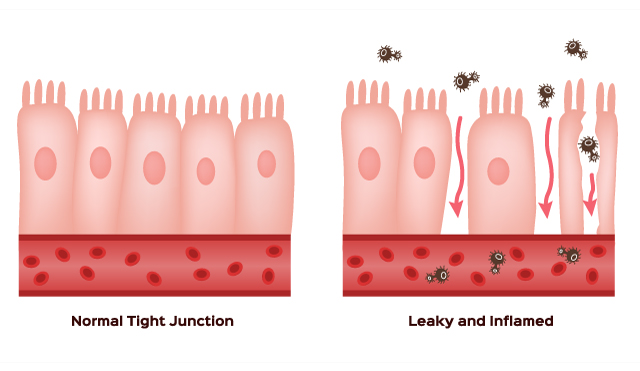
Haver places sleep at the top of her list for a reason. "If you're not sleeping, everything else tends to fall apart," she said. She recommends a cool, dark room and ditching electronics before bed. The goal is to achieve deep sleep, a phase she describes as crucial for cognitive maintenance. "Deep sleep is when your brain, it's like a washing machine … It's washing out all those negative proteins," Haver explained. Missing this restorative phase, she warns, is linked to an increasing risk of dementia, making quality rest a defense against neurological decline.
Fuel with fiber for whole-body wellness
Next, Haver emphasizes a fiber-rich diet, noting a significant gap between intake and need. "Most women get 10 to 12 grams per day," she said. "You need 25 plus, 35 plus [grams] for heart health." This "fibermaxxing" approach supports gastrointestinal and heart health, aids in weight management, and can help prevent diabetes and certain cancers. The benefits are clear, but experts caution that adding fiber should be done gradually to avoid digestive discomfort.
Build strength to preserve independence
The third pillar combines regular movement with intentional strength training. While walking is beneficial, Haver stresses it may not be sufficient. "A lot of women, most of my patients, are walking," she said. "I love walking, but you really need to protect your bones and muscles, and strength training is the quickest and easiest way to do that." This advice is echoed by other health authorities. The U.S. Department of Health and Human Services recommends muscle-strengthening activities at least twice a week to combat age-related muscle loss, or sarcopenia, which begins as early as age 40.
This focus on strength and brain health is driven by a sobering reality Haver calls the "independence gap." While lifespans are increasing, many women face a difficult final decade. "Women by and large are having a rougher go in that last decade and losing their independence," she shared. In her practice, the driving concern has shifted from longevity alone to maintaining autonomy. The fear is losing the ability to live independently, often due to dementia or frailty from lost muscle mass.
The underlying science connects these lifestyle factors directly to the biological shifts of menopause. The decline in estrogen production impacts virtually every system. Cardiologist Dr. Sabeen Chaudry explains, "Estrogen plays an important role in heart health." Its reduction after menopause increases the risk of heart disease, the number one killer of women. Similarly, obstetrician-gynecologist Dr. James Wang notes, "Estrogen is vital to maintaining bone health," with women potentially losing up to 20% of bone mass in the first five years after menopause.
This context makes Haver's three pillars more than just general wellness advice; they are targeted countermeasures. Strength training and calcium intake fight bone density loss. A fiber-rich, balanced diet protects the cardiovascular system. Deep sleep clears the brain. Together, they address the root causes of the independence gap.
Ultimately, the goal is a life not just lived longer, but lived fully. Haver’s patients embody this priority. "They care about staying as healthy and independent as long as possible," she said. "What's the point of living to 120 if you are in a bed and can't take care of yourself?" The message is empowering: the most effective prescription for thriving after menopause may be written not on a pad, but in daily choices about sleep, food, and movement.
Sources for this article include:
Please contact us for more information.