Advertisement
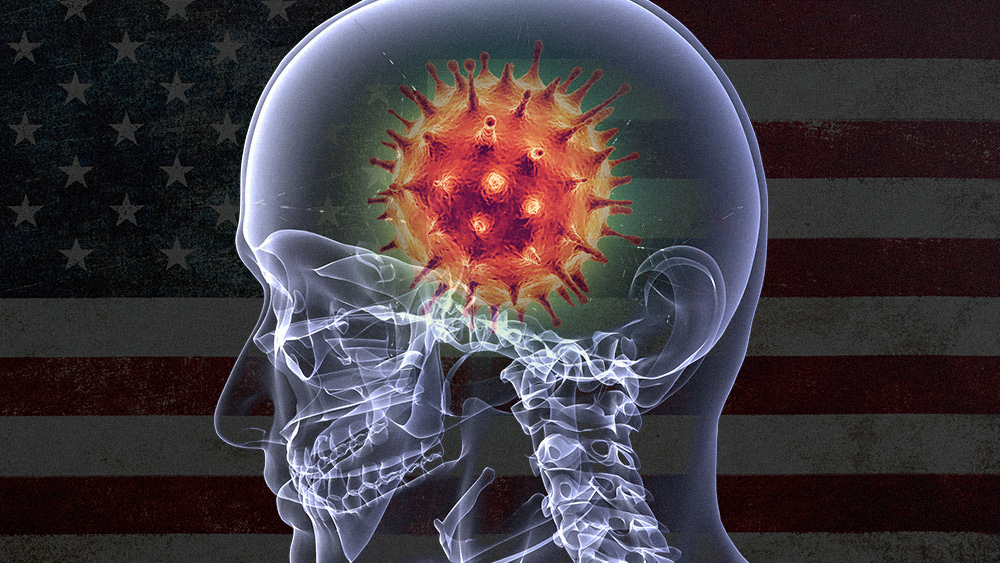
A new review of the infection’s symptoms says that, in addition to the lungs, the Wuhan coronavirus (COVID-19) poses a threat to the entire nervous system.
In the study, published in Annals of Neurology, researchers from Northwestern Medicine noted that about half of hospitalized COVID-19 patients had neurological manifestations of the disease. These included dizziness, headache, muscle pain, decreased alertness, difficulty concentrating, disorders of smell and taste, seizures and stroke.
“It’s important for the general public and physicians to be aware of this, because a SARS-CoV-2 infection may present with neurologic symptoms initially, before any fever, cough or respiratory problems occur,” said lead author Dr. Igor Koralnik, a professor of neurology at Northwestern University Feinberg School of Medicine and chief of neuro-infectious diseases and global neurology at Northwestern Medicine.
COVID-19 has been observed to cause neurological symptoms
Experts have known that the SARS-CoV-2 virus responsible for COVID-19 attacks the nervous system for a while now. Even as early as February, researchers were already looking into the many neurological manifestations of the disease.
In a letter to the editor of the New England Journal of Medicine, a group of Italian doctors noted how some of the COVID-19 patients under their care developed Guillain-Barre syndrome. This neurological disorder sees the patient’s immune system respond to an infection, only for it to mistakenly attack nerve cells, resulting in muscle weakness and even paralysis.
A similar editorial letter, published in Travel Medicine and Infectious Disease, described how COVID-19 patients in China developed encephalitis — the swelling and inflammation of the brain.
A larger study of COVID-19 patients in Wuhan — ground zero for the global pandemic — noted that 36 percent of patients demonstrated neurological manifestations. These ranged from mild symptoms such as headaches and dizziness — likely caused by a robust immune response — to more specific and severe symptoms such as the loss of smell and taste, muscle weakness, seizures, stroke and hallucinations. That same study also noted that these symptoms manifested more often in severe cases of COVID-19, with estimates ranging from 46 to 84 percent. (Related: Yes, it’s REAL: Coronavirus patients are losing their sense of smell and taste – and aren’t getting them back.)
How COVID-19 affects the nervous system
While most of the previous studies have looked at specific neurological manifestations, the Northwestern Medicine review focused on looking at all possible neurological symptoms stemming from COVID-19, as well as how to diagnose them.
Based on what they observed, Koralnik and his team believe that COVID-19 may affect the entire nervous system, including the brain, spinal cord and nerves, as well as the muscles.
As the virus also attacks other organs, such as the lungs, kidneys and heart, the brain may also suffer from lack of oxygenation or from clotting disorders that can lead to hemorrhagic or ischemic strokes.
The virus may also directly infect the brain and the meninges. In addition, the immune system’s reaction to this infection may cause inflammation that can cause nerve and brain damage.
Koralnik and his colleagues have since formed a “Neuro-COVID” research team. The team has started a retrospective analysis of all COVID-19 patients hospitalized at Northwestern Medicine to determine the types of neurological complications they faced, how frequently these complications occurred, as well as how well the patients responded to treatment.
Researchers still looking at long-term effects of the disease
Currently, knowledge about the long term outcome of neurologic manifestations of COVID-19 is limited. To address this, Koralnik and his team will also follow some of Northwestern Medicine’s prospectively in a new outpatient clinic.
The team is looking to determine whether any of the neurological manifestations of the disease is permanent, or if they’re only temporary.
A similar study from France has already identified that changes in consciousness seen in severe COVID-19 cases, such as disorientation, inattention and movement disorders, can persist after recovery.
According to Koralnik, studies like these will provide a foundation for how to diagnose, manage and treat the COVID-19’s many neurologic manifestations.
Sources include:
Advertisement
Advertisements