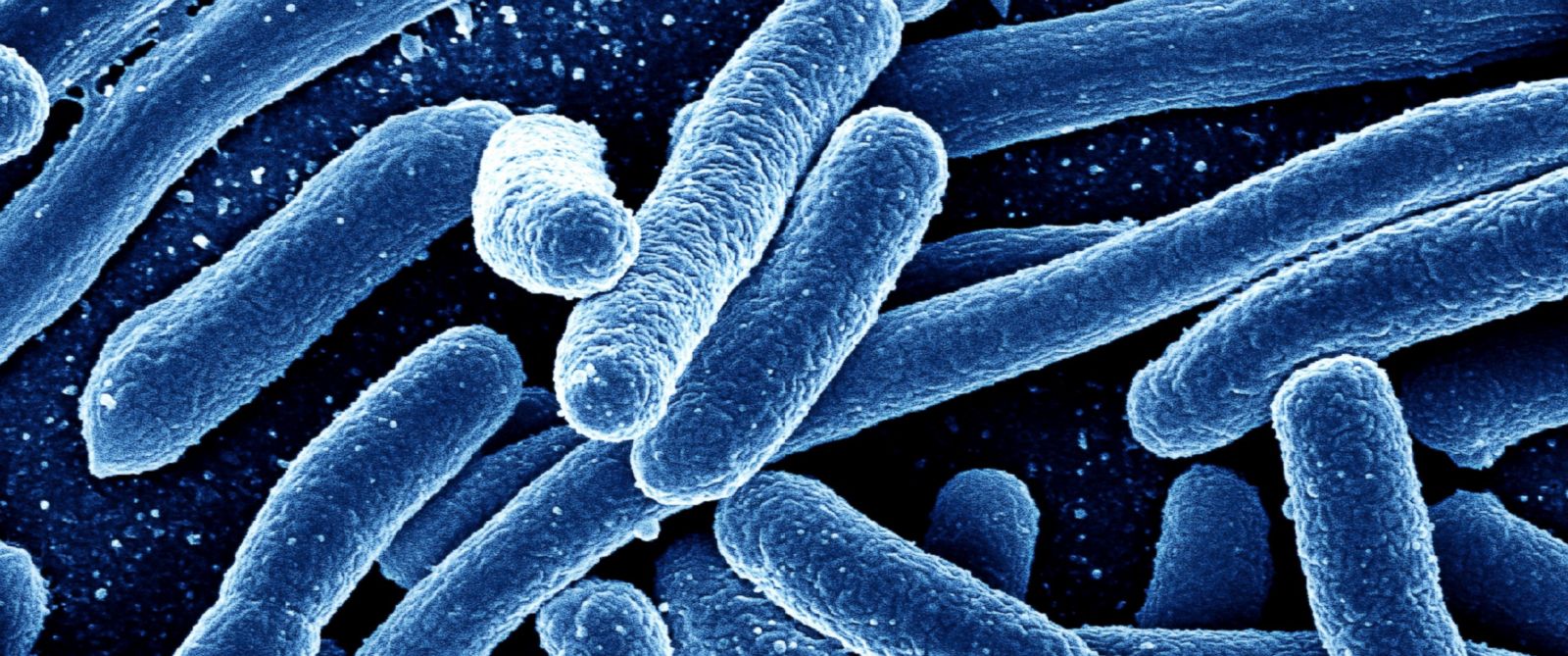
When you think of a pandemic, global disease outbreaks like the Spanish flu that killed 50 million in the early 1900s or the more recent HIV/AIDS pandemic are what usually come to mind. However, some experts are warning that the next pandemic will come from an unexpected source – and it’s something that could largely be prevented if countries take the right precautions now.
The Organization for Economic Cooperation and Development (OECD), which is an advisor to the World Health Organization on initiatives for public health, has warned that public healthcare and spending face “disastrous consequences” if basic hospital hygiene is not improved and antibiotic use isn’t curbed.
The group said that superbugs could kill 2.4 million people by the year 2050; drug-resistant bacteria are already responsible for thousands of deaths, killing more than 33,000 Europeans in 2015 alone. The OECD said that the cost of treating these infections could climb to roughly $3.5 billion, on average, per year in each of the countries analyzed. The group said the countries are already spending around ten percent of their healthcare budget on antimicrobial-resistant bug treatment.
OECD public Health Leader Michele Cecchini said: “AMR costs more than the flu, more than HIV, more than tuberculosis. And it will cost even more if countries don't put into place actions to tackle this problem.”
At the heart of this problem is the overuse of antibiotics, and we're being hit from all angles. Doctors are prescribing antibiotics for viruses, which don’t respond to such medications, and they are also making their way into our bodies through agriculture and livestock products that are given such medications. As a result, many bacteria strains are developing that are able to resist the effects of antibiotics.
Resistance is already incredibly high in lower- and middle-income countries, with as much as 60 percent of the bacterial infections seen in places like Brazil, Russia and Indonesia already resistant to one or more antibiotics. The growth of these infections is expected to be 47 times faster in 2030.
Expert warn that even small kitchen cuts, minor surgeries and infections like pneumonia could turn deadly. The group also expressed concern about resistance to second-line and third-line antibiotics, which they say will swell by 70 percent by the year 2030. These types of antibiotics are supposed to be reserved for worst-case scenarios, but doctors are already using more of them when they should be using less, and that is seeing some of the best emergency options available right now taking a big hit.
How can this superbug pandemic be avoided?
The OECD says that the only way this superbug disaster could be prevented is by implementing widespread changes in healthcare immediately. For example, they stress that healthcare professionals need to make a better effort when it comes to hygiene in hospitals, washing hands regularly and instituting stricter safety rules.
Quicker testing to determine whether infections are viral or bacterial could also make a big difference as antibiotics are completely useless in the former case. Another approach that may be helpful is delayed prescriptions, which entails requiring patients to wait three days before they pick up antibiotic prescriptions. This is approximately the amount of time that a viral infection would take to run its course. In trials of this approach, two thirds of the patients who were given delayed antibiotic prescriptions never ended up collecting their medicine, which means that they did not take any needless antibiotics and exacerbate the problem.
According to Cecchini, such changes could cost as little as two dollars per person each year, paying for itself within a few months in addition to saving billions of dollars and millions of lives by mid-century.
Sources for this article include:
Please contact us for more information.